The nurse residency program at Yale New Haven Health-Bridgeport Hospital is a year-long program that helps new graduate nurses learn about hospital services, gain confidence in their new roles, and offer peer encouragement to one another, with the goal of increasing nurse retention. Most hospitals throughout the country offer a similar program, which consists of monthly classes and a final research project about a topic of interest to the individual nurse related to her specialty. The aim of the project is to make a research-based practice change that will benefit the patient population. Jacquelyn Ferraro and Megan Murphy are two of the hospital’s 75 new nurses, Yale’s biggest cohort ever. The following is their account of their project, which they presented in front of the entire cohort, as well as nurse educators from individual units.
When choosing a topic for our Nurse Residency Project, we didn’t have to think for long before we began to question the seemingly high incidence of necrotizing enterocolitis (NEC) on our unit. Even with limited knowledge of the disorder as new nurses in the Newborn Intensive Care Unit, we could see that far too many babies were suffering from this devastating illness. Soon enough we made it our mission to spend the next year of our practice researching the disorder and what interventions we could bring to our unit to help lower the incidence.
Almost all of the articles we read about NEC in preterm infants compared one thing—breast milk versus formula. Study after study found that six to ten times more preterm babies developed NEC when formula fed versus breastfed. This overwhelming evidence quickly gave us the idea to implement donor breast milk on our unit to help those babies whose mothers weren’t producing a sufficient amount of their own breast milk.
Over the next several months, we worked with our nurse managers, head neonatologists, and members of Mothers’ Milk Bank Northeast to come up with a plan to get donor milk on our unit. It was easy for everyone to see the reasons why it was necessary to initiate its use, but took much time to discuss logistics of storing the milk, ordering it through the computer system, and dispensing it—all to ensure the utmost safety for the preterm babies receiving it.
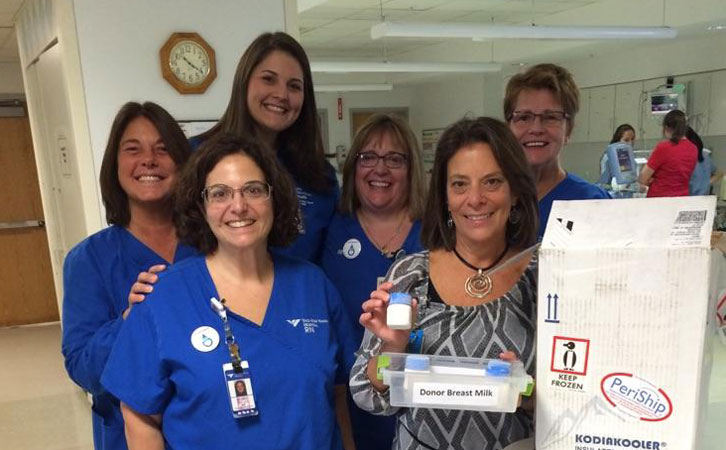
In early September, when we presented our project, entitled “Decreasing the Risk of NEC in Preterm Infants,” we were happy to announce that as of the day before, our NICU had officially implemented the use of donor breast milk, and the first shipment was on its way to the hospital! Not long after, the first baby that qualified for use of the milk was admitted to the unit, and Jacquelyn was lucky enough to be the nurse to provide this vital feeding. The unit continues to get great use out of the donated milk and is looking forward to seeing the evidence of decreased NEC rates over the years to come.
Jacquelyn Ferraro left and Megan Murphy right.










