The NICU – and everything you (likely) didn’t know until now . . .
Perhaps best known for all things back-to-school, September is a big month here at Mothers’ Milk Bank Northeast. Following along here? Or here? Then you may already know that September is also NICU Awareness Month. And with medically fragile infants in more than 100 hospitals (primarily NICUs) across the northeast relying on us to help them grow and thrive, these 30 days are especially dear to us. That’s why we’re busy sharing stories and taking action to both highlight and honor NICU warriors, their families, and all those who help care for them – including our incredible milk donors.
Knowing how much you love a good list (this is still one of our most popular posts) we figured another one was in order. So, get comfortable and get ready to learn everything you didn’t know about the NICU . . .
First up? The basics . . .
Approximately 1 in 10 infants born in the U.S. is admitted to the NICU. That’s about 400,000 babies every single year.
How long a baby remains in the NICU depends on the severity of their illness. While the average stay is said to last 14 days, some little patients require months of specialized care. Remember TyQuell? This adorable warrior (and future linebacker) spent just over eight months in the NICU.
When you think of the NICU, you likely think of preemies – and with good reason. Today, premature birth is the most common reason for a NICU admission. Often smaller with underdeveloped organs and bodily systems, preterm infants are not only at a higher risk for medical complications than their full term counterparts but less “able” to fight off and recover from an illness once it has developed.
That said, there are many other reasons for a NICU stay. Chief among them? Breathing difficulties and all-too-common medical conditions such as jaundice and hypoglycemia.
When it comes to NICU care, there are levels – four to be exact. The American Academy of Pediatrics (AAP) defines these based on babies’ health status, birthweight, and prematurity.
- Level I care is provided in nurseries to low-risk babies – typically those born after 35 weeks.
- Level II care is for “stable or moderately ill” newborns – often those born after 32 weeks’ gestation.
- Level III care typically provides for infants born prior to 32 weeks or weighing less than 3lbs. These babies may require surgery.
- Level IV facilities provide specialized care for the “most complex and critically ill newborn infants.” A full range of pediatric medical and surgical specialists are made available.
Milk? We call it medicine . . .
Breastmilk has well documented benefits (including improved neurodevelopmental, physical, and dental health outcomes) for all babies. However, medically fragile babies being cared for in the NICU, require human milk, which is much more easily tolerated than formula, and actively protects their health. For this reason and more, studies conducted by medical organizations such as the AAP show that when a mother’s own milk is not available, safe donor human milk is the next best option.
In fact, the use of human milk instead of formula, vastly decreases the risk of a premature or very low birth weight (VLBW) baby developing necrotizing enterocolitis – the leading cause of death among preemies after the age of 2 weeks.
Increasingly aware of the importance of human milk, approximately 80% of U.S. based NICUs rely on donor milk to help care for their tiny charges.
And where can this safe, life-saving donor milk be sourced? Often from non-profit milk banks such as Mothers’ Milk Bank Northeast.
Finally – file this under weird but wonderful . . .
Having observed the benefits of warming chambers used to care for baby chicks at the Paris Zoo, French obstetrician Stéphane Tarnier had similar chambers constructed for premature infants under his care. Introduced at L’Hôpital Paris Maternité in 1880, these incubators immediately began saving lives. But with the idea being so new and unusual, few doctors were willing to believe in its life-saving potential.
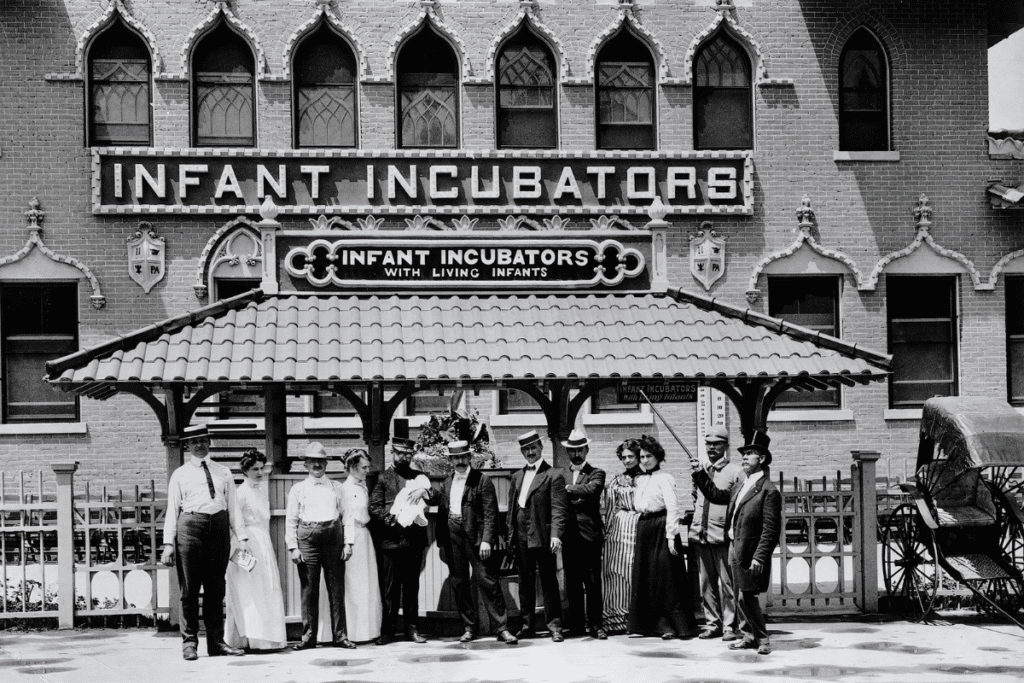
Fast forward several decades and Pierre Budin decided it was time to display the incubators (and several premature babies – remember, different times!) at the Berlin World’s Fair. There, Martin Couney, father of a pre-term daughter, was struck by the success of the exhibit. Realizing people would pay to see doctors and nurses care for these infants, he decided to set up shop in Coney Island.
Starting in 1903, these premature baby exhibits operated much like any other amusement – complete with carnival barkers attempting to lure the public to come see them. As questionable as all this may sound, Couney didn’t charge to take the babies and ticket proceeds were used to care for them. In fact, among the many nurses hired to tend to the infants was his own daughter, Hildegard.
Ultimately, the exhibit ran for decades. In that time, it’s estimated that Couney saw an 85% success rate saving approximately 6,500 little lives. Thankfully, NICU care has come a long way since then. Nevertheless, we’re thankful for every weird-but-wonderful step forward.
Let’s talk!
The NICU is part of the birth story for so many families. Despite this, the experience isn’t widely spoken about or understood. Are you a NICU parent, caregiver, or health professional comfortable sharing your story? We’d love to hear from you. Please feel free to email news@milkbankne.org – any time!