Journalists, providers, and parents often ask us about the differences between, and the risks and benefits of, milk banking and milk sharing.
Milk sharing, including cross-nursing, is not new and not unique to humans; it occurs among other social mammals. It is one aspect of allomothering, or alloparenting, “an adult animal or person involved in parent-like behavior towards an individual that is not his or her offspring.”
Mothers have shared their milk since the beginning of time. For example, when a mother was ill, had died, or was working, another mother might nurse her baby. Over time, women began to pay and be paid to nurse children who were not their own, and wet nursing was born. Slaves were also pressed into wet nursing masters’ babies, often at the cost of their own babies’ health.
Human milk and full-term healthy babies are both robust. Most of the time babies do quite well on another mother’s milk. However, some diseases and medications pass through milk to the baby. This has been known for a long time and wet nursing has been regulated for several millennia. Archaeologists and historians have found wet nursing regulations from ancient Egypt, China, Mesopotamia, and other places.
Commerce—exchange of money for a service or product—is of interest to regulators, for reasons of public safety and collecting taxes. This is why wet nursing was regulated. Sharing of milk in the community, among friends and family members, is private; it has not been, and cannot be, regulated. Education is crucial to safe practice.
Milk sharing and informed choice
For 18 years, parents have the right, privilege, and responsibility to make decisions for their children about their safety, health, education, and so many other things. In the medical world, decisions require informed consent, “permission granted in full knowledge of the possible consequences, typically that which is given by a patient to a doctor for treatment with knowledge of the possible risks and benefits.” Health care providers, sometimes with legal and ethical advice, must decide what information patients, or their parents, need in order to make an informed choice about a procedure, therapy, or medication.
Human milk is both food and medicine. It can be purchased or exchanged without medical involvement. However, the medical and public health communities grapple with their role in informed consent regarding human milk.
What information do parents need to make an informed choice?
- While milk and babies are generally robust, some medications and diseases pass through milk, and can harm the baby.
- Mothers are not always aware that they have these diseases, or that they are taking medications contraindicated for breastfeeding.
- Risk varies depending on the baby’s health and age, especially in the case of prematurity.
- Money matters. Paying for milk increases the risk that it will be diluted or adulterated.
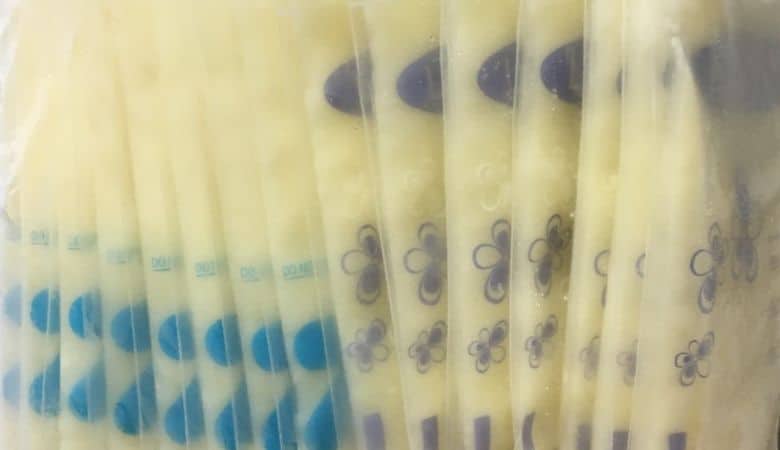
- Shipping milk long distance increases the risk of contamination en route, and therefore requires precautions to ship safely.
What is the responsibility of providers in supporting safe practices?
- Be informed. Be familiar with the relevant scientific and social science research. Risks vary with each baby and situation. Prematurity, overall health, parent input all influence recommendations.
- It is not possible for providers to know everything necessary to care for their young patients. Know where to refer parents for more information and consultation, such as to lactation consultants or breastfeeding medicine physicians.
- Be open to this conversation with parents. There are risks and benefits to using either shared human milk or formula. Families want to look to their providers for informed guidance in this very personal decision, but they are often hesitant to raise the issue, fearing disapproval, admonition, even reporting to Child Protective Services. In its recent Position Statement on Informal Breast Milk Sharing for the Term Healthy Infant, the Academy of Breastfeeding Medicine emphasizes the importance of open informed discussion with patients, rather than a unilateral, almost punitive approach.
What is the role of the public health community in information and safe practice?
- Widely and creatively disseminate accurate, evidence based, linguistically and culturally appropriate information.
- Ensure that practitioners have the necessary tools and education to promote breastfeeding.
- Engage in and promote research on safe, effective use of donor milk and shared milk to support breastfeeding.
Milk sharing, and in the last century, donor milk, have always been part of normal breastfeeding. It is time to reopen thoughtfully and responsibly the conversation about the role of safe donor milk and milk sharing in supporting breastfeeding.