The third week of National Breastfeeding Month focuses on infant and young child feeding in emergencies. Milk bank Executive Director Naomi Bar-Yam provides an overview of the importance of supporting breastfeeding during COVID-19, including evidence from major medical organizations.
Emergencies come in many shapes and sizes. Likewise, feeding infants and children in those emergencies.
On one end of the spectrum are personal and family emergencies—preterm birth, maternal illness, maternal death, and mother and child separation, short or longer term, for any of many reasons. Historically, such emergencies have been resolved close to home. Family, friends, community members took over feeding, nursing, caring for baby. In more recent history, of course, formula filled the role of local and family nursers. Today, family and friends from near and far sometimes offer their milk. Milk banks also provide donor milk in such emergencies.
There are also regional emergencies—natural disasters such as hurricanes, earthquakes, and floods, and man-made disasters such as war and ethnic violence. These result in widespread social disruption, family separation, homelessness, and scarcity of food, water, and electricity. In these emergencies, government agencies and humanitarian organizations are among the first responders, arranging for safe spaces, medical care, and supplies, which often include diapers, clothing, and infant formula, and rarely if ever include breastfeeding information and support. In such emergencies formula and donor milk require water and refrigeration that are likely unreliable and scarce, if they are available at all.
Breastfeeding requires none of these resources. Humanitarian aid includes medical personnel who should be trained in basic breastfeeding education and support. AAP, WHO, and USBC offer helpful guidelines for medical and emergency personnel and parents regarding the importance of and guidelines for breastfeeding in emergencies.
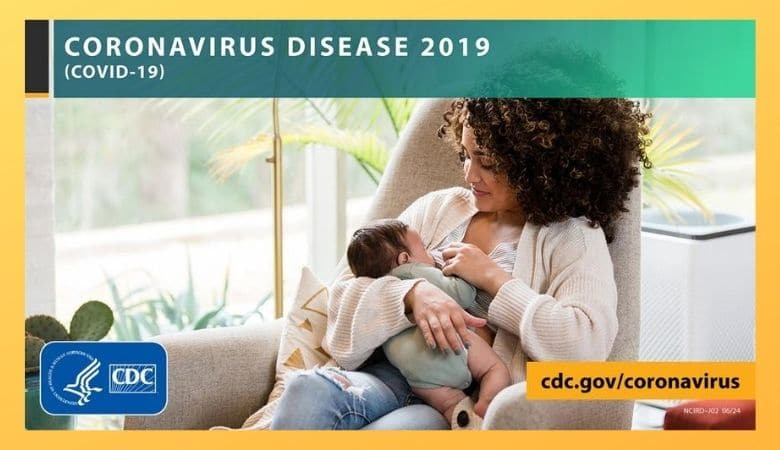
Facts about COVID-19 and human milk
Today, we face a global emergency that is unlike other emergencies. COVID is a new disease. There is much we do not know, though we learn more week by week. The public health community works to give the best advice and guidelines possible, and update them as new information and research indicate.
We know that:
- Human milk contains antibodies to protect babies and help their immature immune systems to develop.
- Breastfeeding keeps mothers and babies close—another form of protection.
- “Active COVID-19 (virus that can cause infection) has not, to date, been detected in the breastmilk of any mother with confirmed/suspected COVID-19”[1].
- COVID virus that may be found in pumped milk is killed in pasteurization[2], making milk from a milk bank safe for use in hospital or at home as needed to support breastfeeding and infant care.
- COVID is contracted in the lungs and is transmitted through droplets exhaled when breathing, coughing, and sneezing, and possibly also through the digestive tract[3],[4].
Breastfeeding with COVID-19
Major medical (AAP, AAFP, ACOG, USBC) and health organizations (WHO) have used our growing knowledge about COVID-19 and similar viruses to make clear recommendations to guide new parents in making informed decisions about infant feeding:
- Women with COVID-19 can breastfeed. They should:
- Wear a mask when they are holding and nursing the baby.
- Wash hands before touching the baby.
- Routinely clean and disinfect surfaces, particularly high-contact surfaces.
- Close contact and early, exclusive breastfeeding help a baby to thrive. A woman with COVID-19 should be supported to breastfeed safely, hold her baby skin-to-skin, and share a room with her baby.
- If a woman with COVID-19 is too unwell to breastfeed, she can be supported to provide her baby with breastmilk in other ways, including by expressing milk, relactation, donor human milk.
None of these is, of course, medical advice for any individual mother/baby. They are, rather evidence-based guidelines to inform parents’ decisions and conversations with their health care providers in their personal situations.
Decades of breastfeeding and human milk research, education, and advocacy have helped to normalize breastfeeding. Medical and public health organizations are not defaulting to formula at the first sign of trouble. They are researching and educating about safe ways to breastfeed. It is National Breastfeeding Month 2020. In this time of crisis, let’s take a moment to notice and celebrate this achievement.
[1] World Health Organization Frequently Asked Questions: Breastfeeding and COVID-19 for Health Care Workers. 12 May 2020. Accessed 2 August, 2020.
[2] Unger S. et al. Holder pasteurization of donated human milk is effective in inactivating SARS-Cov-2. CMAJ 2020. doi: 10.1503/cmaj.201309; early-released July 9, 2020
[3] Hubrecht Institute. “Coronavirus SARS-CoV-2 infects cells of the intestine.” ScienceDaily. ScienceDaily, 4 May 2020. <www.sciencedaily.com/releases/2020/05/200504091438.htm>. Accessed 2 August, 2020
[4] Yang, L and Tu, L. Implications of Gastrointestinal Manifestations of COVID -19. The Lancet.com/gastrohep. 12 May 2020 https://doi.org/10.1016/ S2468-1253(20)30132-1 . Accessed 2 August, 2020